How does healthcare revenue generation impact patient care and financial stability? Understanding the critical role of revenue cycle management.
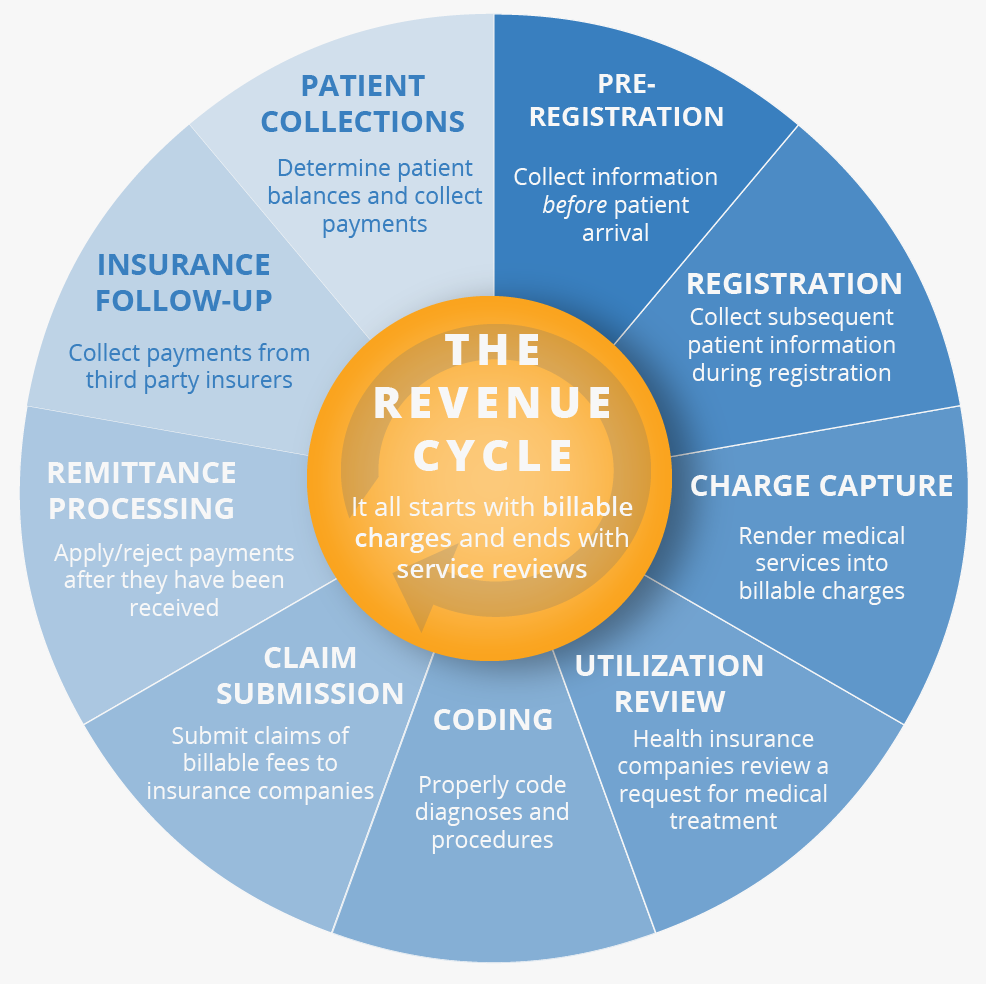
The process of converting patient services into cash is a fundamental aspect of healthcare operations. This encompasses all activities from initial patient encounter to final payment collection. Key steps include billing, coding, insurance verification, and accounts receivable management. Effective management of this process is crucial for maintaining financial stability and ensuring resources are available for patient care. For example, a smoothly functioning revenue cycle enables a hospital to consistently and predictably collect payments, allowing it to meet operating expenses and invest in new technologies or staff.
Efficient revenue cycle management offers numerous benefits. It reduces administrative costs by streamlining processes and minimizing errors. Improved cash flow allows healthcare organizations to invest in better equipment, technology, and staffing. This, in turn, leads to improved patient care outcomes. Furthermore, a robust system enhances the organization's financial stability, reducing the risk of operational disruptions due to insufficient funds. This has become increasingly critical in today's complex healthcare environment, where financial sustainability is essential for the long-term health and vitality of any institution.
- Best Prl Insurance Quotes Coverage Get A Free Quote Now
- Charming Alturas California Explore The High Sierra
Moving forward, we'll delve deeper into specific strategies for optimizing the various stages of this critical process. Topics include enhancing claims processing, improving patient communication, and implementing effective debt collection strategies.
Revenue Cycle
Effective revenue cycle management is paramount to healthcare financial stability. Accurate billing, timely collections, and streamlined processes are essential for sustainable operations and patient care.
- Billing accuracy
- Claims processing
- Patient communication
- Insurance verification
- Accounts receivable
- Coding compliance
- Payment posting
- Denial management
These key aspects, taken together, form a complete revenue cycle. Billing accuracy, for example, prevents costly errors that delay or deny payments. Efficient claims processing ensures timely reimbursements. Effective communication with patients and insurance providers minimizes denials and facilitates timely payments. Strong accounts receivable management collects outstanding balances, ultimately impacting cash flow. Coding compliance ensures claims are processed accurately and in accordance with regulations. Accurate payment posting ensures correct financial recording. Denial management proactively addresses payment denials, avoiding financial losses. All these elements contribute to maximizing revenue generation and ensuring financial sustainability within healthcare institutions. Their interconnectedness creates a cycle that, when optimized, allows institutions to dedicate more resources to patient care.
1. Billing Accuracy
Accurate billing is fundamental to a healthy revenue cycle. Inaccurate billing directly impacts the collection of payments owed, which, in turn, significantly affects a healthcare organization's financial health. Errors can lead to delayed or denied claims, resulting in substantial losses in revenue and operational efficiency.
- Accurate Coding and Procedure Reporting
Correctly identifying and reporting procedures and diagnoses is essential. Incorrect coding can lead to claims being rejected by payers, resulting in lost revenue. Careful review of medical records, compliance with relevant coding guidelines, and regular training for billing staff are crucial for maintaining accuracy. A missed or incorrectly reported procedure, for instance, can severely impact the revenue cycle, as it can prevent payment for a service rendered.
- Precise Insurance Information and Eligibility Verification
Accurate insurance information ensures claims are submitted to the correct payer. Ensuring eligibility status, benefits, and coverage limits are precisely verified is vital. A missed or incorrect insurance detail can result in claims being denied or the payment amount reduced. Employing automated insurance verification systems and regularly updating payer contracts can minimize these errors.
- Comprehensive and Accurate Documentation
Thorough documentation of services performed and patient details directly supports accurate billing. This documentation should meticulously reflect the care provided. Inaccurate or incomplete documentation can hinder timely claim processing. Maintaining a complete, accurate, and verifiable record of the patient encounter is critical to accurate billing and subsequent revenue collection.
- Effective Internal Review and Quality Control Measures
Regular internal reviews and audits of billing processes help catch errors before they impact patient accounts and payers. This includes a comprehensive review of billing procedures and adherence to established guidelines and compliance procedures. This measure is pivotal to ongoing revenue cycle optimization by preventing errors that lead to loss of revenue. A rigorous system of internal checks helps identify and rectify potential discrepancies.
Maintaining billing accuracy throughout the revenue cycle is critical. Consistent, systematic accuracy efforts reduce denials, improve claim processing times, and bolster the overall revenue cycle performance. By mitigating errors, healthcare organizations can enhance financial stability and streamline the process of converting services into cash, thereby optimizing their revenue cycle.
2. Claims Processing
Claims processing is a critical component of the revenue cycle. Accurate and timely processing of claims directly impacts the financial health of healthcare organizations. Efficient claims handling minimizes delays in receiving payments from insurance companies, ensuring a steady flow of revenue and ultimately supporting the overall financial stability of the organization.
- Accurate Coding and Documentation
Precise coding and comprehensive documentation are paramount. Correctly identifying procedures and diagnoses using appropriate medical codes ensures claims are processed accurately and promptly. Inaccurate coding can result in claims being denied or processed incorrectly, leading to delays and revenue losses. Detailed and verifiable medical records are indispensable for accurate claim processing. For instance, a missing or incorrect code for a surgical procedure can halt payment. Careful attention to detail at this stage is crucial for maintaining a robust revenue cycle.
- Insurance Verification and Eligibility
Validating insurance information and confirming eligibility before submitting claims minimizes denials and ensures payment processing aligns with the patient's coverage. Prompt verification of coverage details, including benefits and limitations, is vital. Failure to accurately verify insurance information can result in claim rejection or payment reductions, jeopardizing the revenue cycle. For example, an out-of-network provider lacking updated insurance eligibility for the patient can lead to delays and denials.
- Efficient Claim Submission and Tracking
Streamlined submission processes and robust tracking systems minimize delays. Utilizing automated claim submission systems and establishing a clear process for tracking the status of submitted claims are vital for efficient management of the revenue cycle. Timely tracking of claim status allows for proactive identification and resolution of potential issues. This enables the revenue cycle management team to address issues like missing information before claims are denied, preventing delays and maximizing reimbursement potential.
- Denial Management and Resolution
Addressing claim denials proactively minimizes revenue loss and improves the revenue cycle's efficiency. Effective strategies for identifying and resolving claim denials are essential. A dedicated denial management process, coupled with a comprehensive system for identifying and correcting errors, is necessary. Prompt responses to claim denials by investigating reasons for rejection and correcting errors reduces overall delays in payment. For example, a denial due to missing signatures on forms can be corrected quickly, minimizing impact on the revenue cycle.
Effective claims processing, encompassing accurate coding, insurance verification, efficient submission, and proactive denial resolution, is intrinsically linked to the overall health of the revenue cycle. By optimizing these aspects of claims processing, healthcare organizations can strengthen their financial position and maintain a steady flow of revenue, which, in turn, supports improved patient care.
3. Patient Communication
Effective patient communication plays a crucial role in optimizing the revenue cycle. Clear and timely communication regarding appointments, procedures, billing, and payment options directly impacts the efficiency and accuracy of the revenue cycle. Poor communication can lead to delayed payments, increased administrative burden, and ultimately, financial strain.
- Appointment Scheduling and Reminders
Clear and readily accessible appointment scheduling tools, coupled with automated reminders, reduce no-shows and missed appointments. This minimizes wasted resources and contributes to the overall efficiency of the revenue cycle. Failure to communicate effectively about appointment rescheduling or cancellations can lead to complications. For example, an automated reminder system can help minimize cancellations and no-shows, avoiding lost revenue opportunities due to unfilled appointments.
- Explanation of Procedures and Costs
Comprehensive information about medical procedures, including associated costs and payment options, fosters transparency and understanding. This reduces the likelihood of misunderstandings regarding charges and facilitates a smooth payment process. Lack of clarity can lead to disputes and delays in payment. For example, pre-authorization and estimated cost information provided proactively can minimize disputes and encourage timely payments.
- Clear Billing and Payment Information
Providing patients with detailed billing statements and clear instructions for making payments enhances the likelihood of timely payments. This can include multiple payment options and easy-to-understand payment schedules. Failure to explain billing procedures or provide clear payment instructions can lead to confusion and delays. For example, offering online payment portals and automated statements enhances patient convenience and accelerates payment processing.
- Addressing Concerns and Complaints
Establishing clear channels for patients to express concerns or complaints facilitates resolution and minimizes disputes. Prompt and effective responses to inquiries and complaints lead to greater patient satisfaction and fewer disputes about billing. A lack of responsiveness or inadequate resolution channels can lead to escalated issues and financial challenges. For example, a dedicated customer service department or online portal for resolving billing questions streamlines the process for both patients and administrative staff, minimizing financial losses.
Effective patient communication acts as a critical link between the healthcare provider and patient. These strategies, when effectively implemented, reduce administrative burdens, minimize disputes, and promote timely payment collection. In turn, they support a more efficient and financially sound revenue cycle, ultimately benefiting all stakeholders.
4. Insurance Verification
Accurate insurance verification is intrinsically linked to the revenue cycle's effectiveness. The process of confirming a patient's insurance coverage, benefits, and eligibility directly impacts the financial viability of healthcare organizations. Correctly identifying and verifying insurance information is critical for proper billing and timely payment collection, ultimately influencing the organization's financial health. A streamlined and accurate verification process ensures claims are submitted to the correct payer, reducing the likelihood of denials and maximizing reimbursement. Inaccurate or incomplete verification often results in delayed payments or claim rejection, causing significant revenue loss and administrative burden. For instance, a hospital that fails to verify a patient's insurance coverage before performing procedures faces potential losses due to unpaid claims and the necessity of handling appeals and denials.
The importance of insurance verification extends beyond simple cost recovery. Accurate verification ensures compliance with payer regulations and contractual agreements. Denials stemming from incorrect or incomplete information can result in penalties and legal issues for healthcare providers. Proper verification also helps streamline the claims process, reducing processing time and administrative costs. A smooth and effective verification process directly correlates with a more efficient revenue cycle, minimizing claim denials and enhancing cash flow. The prompt verification of a patient's coverage for a specific procedure, for example, avoids delays in reimbursement, thereby enhancing the financial stability of the healthcare entity. This, in turn, allows for better allocation of resources to patient care and operational improvements.
In summary, insurance verification is a cornerstone of a robust revenue cycle. Its impact extends beyond immediate financial gains. Accurate and timely verification reduces claim denials, minimizes administrative costs, and promotes compliance with payer regulations. Understanding the interplay between insurance verification and the revenue cycle is crucial for the financial well-being and long-term sustainability of healthcare organizations. Effective implementation of accurate and efficient insurance verification protocols strengthens the revenue cycle, enabling healthcare providers to allocate more resources to patient care and maintain financial stability.
5. Accounts Receivable
Accounts receivable (AR) is a crucial component of the revenue cycle, directly impacting financial stability and operational efficiency in healthcare and other industries. AR represents the total amount owed to an organization for goods or services delivered but not yet paid for. A strong and well-managed AR process is integral to a healthy revenue cycle, as it directly affects cash flow. Effectively managing AR contributes to prompt revenue collection, enabling organizations to meet obligations and invest in future growth. Conversely, poor AR management can lead to significant financial strain and hinder operational efficiency. Delinquent accounts tie up capital, impacting the organization's ability to invest in equipment or personnel. For example, a hospital experiencing high levels of outstanding AR payments might be forced to postpone essential equipment upgrades, impacting patient care.
The connection between AR and the revenue cycle is undeniable. AR management directly influences the revenue cycle's overall performance. A well-structured AR process involves accurate billing, timely follow-ups with patients or insurers, proactive collection strategies, and clear communication regarding payment options. These elements translate into a smoother and more predictable revenue stream. By minimizing the number of outstanding invoices, organizations ensure a more efficient and reliable revenue stream. For example, a clinic with a highly efficient AR department will see a more consistent and predictable cash flow, allowing for better planning and budgeting. Conversely, an inefficient AR department might see significant fluctuations in cash flow, potentially hindering the clinic's ability to effectively respond to financial demands or investment opportunities. This highlights the critical role of AR in ensuring the financial health and operational effectiveness of an organization.
Effective accounts receivable management is essential to a healthy revenue cycle. A strong understanding of the interplay between AR and the revenue cycle is vital for sustainable operational effectiveness. Organizations must recognize that timely and accurate collection of payments directly supports their financial stability. By implementing proactive measures, such as clear payment terms, automated reminders, and a dedicated collections department, organizations can optimize their AR management and contribute to a thriving revenue cycle. Ultimately, efficient AR management ensures organizations can maintain resources for operations and service delivery while simultaneously strengthening their financial position. This, in turn, fosters improved service quality and sustainability across diverse sectors.
6. Coding Compliance
Accurate medical coding is fundamental to a robust revenue cycle. Correctly assigning codes ensures accurate billing and reimbursement, directly impacting a healthcare organization's financial health. Noncompliance with coding guidelines can lead to claim denials, rejected payments, and, ultimately, significant financial losses. Understanding the intricate relationship between coding compliance and the revenue cycle is crucial for optimizing financial performance and ensuring sustainable operations.
- Accurate Coding and Reimbursement
Accurate coding directly translates into accurate reimbursement. Precise application of coding guidelines ensures claims are processed correctly, leading to prompt and full payments from insurance providers. Errors in coding, such as incorrect procedure codes or inaccurate diagnosis codes, result in claim denials. These denials can have substantial financial repercussions for a healthcare entity, negatively impacting its ability to meet operational expenses.
- Compliance with Regulatory Requirements
Healthcare organizations are subject to various regulatory requirements regarding medical coding. Noncompliance can lead to severe penalties, including fines and legal action. These penalties erode financial resources and can damage a facility's reputation, further impacting its revenue cycle. Strict adherence to coding guidelines and regulations, therefore, safeguards the organization from financial and legal issues.
- Minimizing Claim Denials
Correct coding significantly reduces claim denials. Denials result from a variety of coding errors, from incorrect procedure codes to missing or incomplete documentation. A dedicated effort to maintain accurate coding procedures can directly prevent denials, thereby ensuring a smoother and more reliable revenue stream. An optimized coding system effectively manages these challenges, allowing for a higher reimbursement rate and a stable revenue cycle.
- Maintaining Consistent Revenue Streams
Precise coding supports a consistent revenue stream, critical for long-term financial stability. Fluctuations in revenue due to coding errors can disrupt financial planning and create uncertainties in meeting operational costs. Coding compliance establishes a predictable revenue stream that enables the organization to operate more efficiently and effectively. Maintaining this predictability minimizes financial risks and strengthens financial planning capabilities.
In conclusion, coding compliance is not merely a regulatory requirement but a crucial component of a well-functioning revenue cycle. By ensuring accuracy in medical coding, healthcare organizations minimize claim denials, maximize reimbursement, and create a stable revenue stream. This directly contributes to the financial stability and long-term sustainability of the organization, underpinning its ability to effectively address operational expenses and improve patient care.
7. Payment Posting
Payment posting is a critical step in the revenue cycle, representing the formal recording of payments received. This process links financial transactions to patient accounts, ensuring accurate reflections of cash flow and facilitating accurate financial reporting. Its importance stems from its direct impact on revenue recognition, accounts receivable management, and overall financial stability of healthcare organizations.
- Accuracy and Timeliness
Accurate and timely posting is paramount. Errors in posting can lead to discrepancies in financial records, impacting reconciliation processes and potentially leading to audit issues. Delayed posting can also impact cash flow, delaying the organization's ability to meet operational expenses. An example of this is a mismatched transaction amount or incorrect date in the payment ledger, which would distort financial reports and make reconciliation efforts more complex and prone to error.
- Matching and Reconciliation
Payment posting must be meticulously matched to corresponding invoices, claims, and patient accounts. This matching ensures that payments are credited to the correct accounts, preventing discrepancies and contributing to a more accurate portrayal of cash flow. Failure to reconcile payments with billing records can lead to significant challenges in account management and financial reporting. A real-world scenario includes the reconciliation of a check payment with the corresponding patient account and invoice, confirming both details align before recording the transaction. An unverified posting can lead to an erroneous account balance and potentially delayed cash flow.
- Auditing and Compliance
Thorough payment posting practices are essential for meeting regulatory requirements and facilitating smooth auditing processes. Proper documentation and sequential recording of payments ensures traceability and compliance with accounting standards and regulations. Non-compliance in payment posting procedures can result in regulatory sanctions and penalties for the organization. A hospital's payment posting system, for instance, must be able to demonstrate the traceability of each payment, supporting accurate and transparent financial reporting.
- Impact on Cash Flow Management
Accurate and timely payment posting directly affects cash flow. The speed at which payments are posted and reconciled influences an organization's ability to meet short-term and long-term financial obligations. A well-optimized payment posting system allows for immediate reconciliation and facilitates improved financial forecasting, enabling more precise financial planning. A hospital's immediate access to funds generated from posted payments allows for the timely allocation of resources, thereby supporting seamless operations.
In summary, payment posting is not simply a clerical function; it is a pivotal component of the revenue cycle. Its accuracy, timeliness, and meticulous matching with other financial transactions significantly contribute to a robust revenue cycle management process. Effective payment posting safeguards financial integrity, enables accurate reporting, and ultimately supports a financially sound healthcare organization. This aspect of the revenue cycle directly impacts the ability of organizations to maintain operational efficiency, meet financial obligations, and provide high-quality patient care.
8. Denial Management
Denial management is a critical component of the revenue cycle. It focuses on identifying and resolving denials of insurance claims. Denials occur when insurance providers reject a claim for payment, often due to discrepancies in billing, coding, or documentation. Effective denial management directly affects the financial health of healthcare organizations. The inability to efficiently resolve denials translates to lost revenue, negatively impacting the organization's cash flow and ability to meet its operational expenses. This lost revenue directly impacts the revenue cycle's overall efficiency and financial sustainability.
The process involves meticulous review of the denied claim, identification of the reason for denial, and subsequent resubmission of the claim with corrections. This process may involve correcting coding errors, clarifying documentation issues, or appealing the denial to the insurance provider. Effective denial management strategies encompass a proactive approachpreventing errors that lead to denials in the first placeand a reactive approachswiftly resolving denied claims. Comprehensive training for billing and coding staff, along with robust internal review processes, are essential in minimizing denial rates. For instance, a hospital with a proactive denial management system that quickly resolves coding discrepancies experiences a more consistent and predictable revenue stream, enabling more reliable financial planning and ultimately supporting better patient care. Conversely, a lack of a structured denial management process leads to a higher rate of claim denials, resulting in significant revenue losses and operational inefficiencies. This loss in revenue can severely impact the organization's budget and the ability to fund essential services.
In summary, denial management is not simply a corrective measure but a crucial proactive and reactive process. By effectively identifying, analyzing, and resolving claim denials, healthcare organizations can significantly improve their revenue cycle. Understanding the interplay between denial management and the revenue cycle is vital for ensuring financial stability and optimizing the efficient conversion of services into revenue. Comprehensive denial management systems support the smooth functioning of the entire revenue cycle by minimizing claim rejection rates, maximizing reimbursement potential, and ultimately bolstering the organization's financial health and patient care initiatives.
Frequently Asked Questions
This section addresses common questions and concerns regarding revenue cycle management in healthcare settings. Comprehensive understanding of these processes is crucial for financial stability and operational efficiency.
Question 1: What is revenue cycle management (RCM)?
Revenue cycle management encompasses all activities involved in converting patient services into cash. It encompasses the entire process, from initial patient contact to final payment collection. This includes billing, coding, insurance verification, accounts receivable management, and claims processing. Effective RCM maximizes revenue and ensures financial sustainability.
Question 2: Why is RCM important for healthcare organizations?
RCM is critical for healthcare organizations' financial stability. Efficient processes ensure timely revenue collection, reducing the risk of cash flow issues. A well-managed revenue cycle allows institutions to meet operational expenses, invest in equipment and technology, and ultimately support quality patient care. Strong financial stability directly supports healthcare organizations' long-term viability and their capacity to provide essential services.
Question 3: What are common challenges in RCM?
Common challenges include coding errors, inaccurate billing, insurance claim denials, complex payer regulations, and inefficient accounts receivable processes. These issues can lead to significant revenue loss, operational inefficiencies, and financial strain.
Question 4: How can organizations improve their RCM processes?
Organizations can enhance their RCM processes through various strategies. These include accurate coding, streamlined billing procedures, effective insurance verification, proactive denial management, and robust accounts receivable practices. Implementing advanced technologies and employing experienced personnel can further optimize these processes.
Question 5: What is the impact of technology on RCM?
Technology plays an increasingly significant role in RCM. Automated systems for billing, claims processing, insurance verification, and patient communication streamline workflows and reduce errors. Electronic health records (EHRs) and other digital tools improve data accuracy and facilitate faster claim processing, which directly impacts the organization's ability to collect payments and maintain a stable financial position.
A well-structured and managed revenue cycle is paramount to financial sustainability and ultimately, the quality of patient care in a healthcare setting. These FAQs offer basic insight into this complex area.
Next, we'll examine specific strategies for optimizing the various stages of the revenue cycle.
Conclusion
This exploration of revenue cycle management highlights the critical role this process plays in the financial sustainability and operational effectiveness of healthcare organizations. Key components, including accurate billing, efficient claims processing, effective patient communication, robust insurance verification, sound accounts receivable management, precise coding compliance, streamlined payment posting, and proactive denial management, collectively determine the success of the revenue cycle. Each stage, when optimized, contributes to a more predictable and reliable revenue stream, enabling organizations to meet operational expenses and invest in patient care improvements. Failure to address these processes effectively can lead to substantial financial strain, impacting resource allocation and ultimately the quality of care provided.
Maintaining a healthy revenue cycle is not merely a financial concern but a fundamental aspect of healthcare provision. Optimizing these processes is crucial for long-term viability and sustainability. Healthcare organizations must prioritize continuous improvement in revenue cycle management. This involves ongoing evaluation of existing processes, proactive implementation of technological advancements, and a commitment to fostering a culture of accuracy and efficiency throughout the entire cycle. The future of healthcare necessitates a robust and reliable revenue cycle to maintain financial stability, promote innovation, and ultimately, deliver high-quality patient care.