Understanding the Critical Dosage: A Vital Concept in Medicine
A crucial aspect of medication administration is the precise dosage required to achieve therapeutic effects. This optimal dose, often significantly lower than the maximum tolerated level, is frequently employed in clinical settings and crucial for patient safety. This prescribed amount, while necessary to treat, minimizes potential harm and ensures efficacy. It's a delicate balance, as exceeding this dose can be detrimental.
The concept refers to the minimum effective concentration or amount of a medication needed to produce the desired therapeutic effect. It's frequently utilized in clinical trials to determine the suitable dose range for a given treatment. Determining the optimal medication dose is a multifaceted process encompassing factors such as the individual patient's characteristics, the specific condition being treated, and the drug's potential side effects. A lower, effective dose reduces the risk of unwanted consequences. Historically, the identification of this optimal dosage has been a cornerstone of pharmaceutical development and medical practice, playing a significant role in reducing adverse events and improving patient outcomes.
This understanding of dosage is fundamental to various medical specialties, from oncology and cardiology to psychiatry. Specific examples of this principle are seen in the nuanced approaches to treating conditions such as cancer, where precise medication administration is critical. From optimizing the efficacy of therapies to ensuring their safety, knowledge of this principle is vital in modern medicine.
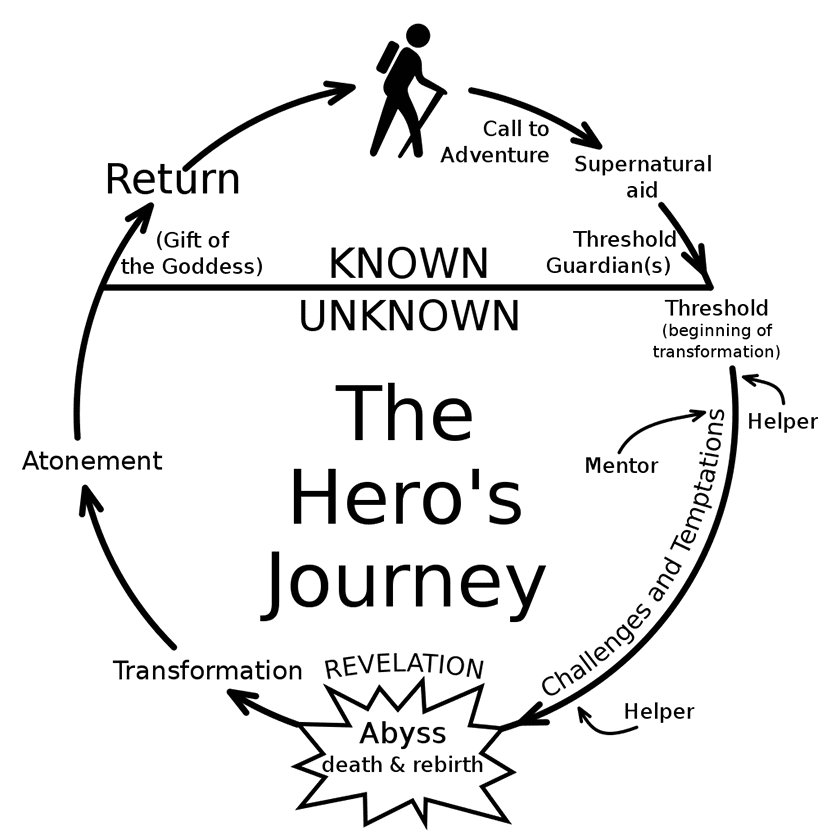
Hero's Dose
The "hero's dose" is a critical concept in medicine, emphasizing the precise and often minimal dosage required for therapeutic effect. Understanding its various facets is essential for effective treatment and minimizing adverse reactions.
- Optimal dosage
- Therapeutic effect
- Patient safety
- Reduced toxicity
- Clinical trial design
- Individualized treatment
- Drug efficacy
- Minimizing side effects
These aspects highlight the delicate balance between achieving desired outcomes and preventing harm. Optimal dosage, for instance, focuses on the lowest effective level, maximizing therapeutic effect while minimizing toxicity. Patient safety is paramount, as treatment must be carefully tailored to individual characteristics. Clinical trial design often utilizes this principle to identify the most effective and safest dose range. Drug efficacy is directly tied to the appropriate dose. Individualized treatment acknowledges variations in patient responses to medications, emphasizing tailored dosage regimens for optimal results. Understanding these facets, including how they interrelate, is essential for progress in medical practice and patient care.
1. Optimal Dosage
Optimal dosage, a core concept in pharmacology, directly relates to the "hero's dose" by representing the precise, minimal amount of medication required to achieve a therapeutic effect. This minimum effective dose minimizes potential side effects and maximizes the desired therapeutic response. The goal is to find the sweet spot between efficacy and safety. A drug's therapeutic index, the ratio of the toxic dose to the therapeutic dose, underscores the importance of precise dosage; a wider index indicates a greater safety margin, allowing for a wider range of effective doses. For instance, in treating certain cancers, administering the optimal dose of chemotherapy drugs allows for successful tumor reduction while limiting the debilitating side effects that can diminish patient quality of life. Precision in dosage ensures that treatment is efficacious without undue harm.
Furthermore, the concept of optimal dosage underpins the selection and administration of medication in various clinical settings. Clinical trials meticulously evaluate the optimal dosage range to ensure safety and efficacy across a diverse patient population. Careful consideration of factors such as age, weight, pre-existing conditions, and the specific condition being treated are crucial to achieving an optimal dosage. The use of biomarkers and pharmacogenomics is increasingly utilized to tailor treatment and dosage regimens, potentially leading to a more personalized approach to medication administration. This precision-dosing approach allows clinicians to precisely administer the optimal dosage, which is a key part of the "hero's dose" concept. Consequently, treatment outcomes improve while the risk of adverse effects decreases. Examples range from managing diabetes with precise insulin doses to treating infections with tailored antibiotic regimens. A well-defined optimal dosage enhances the likelihood of a successful therapeutic outcome and minimizes the likelihood of harmful side effects.
In summary, optimal dosage is fundamental to the "hero's dose" concept. Precisely determining the optimal dose is not merely about achieving a therapeutic effect but also about mitigating potential harm. The pursuit of this optimal dose is a cornerstone of modern medicine, driven by a commitment to patient safety and therapeutic success. While challenges such as inter-individual variability and drug interactions persist, continued research in pharmacokinetics and pharmacodynamics, coupled with advanced diagnostic tools, promises further refinement in the determination and application of optimal dosages, enabling even more effective and safer treatment approaches. This will, in turn, reinforce the vital link between "optimal dosage" and the therapeutic efficacy of treatment regimens.
2. Therapeutic Effect
The therapeutic effect, a fundamental aspect of medical treatment, directly correlates with the concept of the "hero's dose." A medication's therapeutic effect refers to the desired positive outcome resulting from its administration. The "hero's dose," conversely, represents the precise amount of medication necessary to achieve this effect while minimizing adverse reactions. Crucially, the strength of the therapeutic effect is intrinsically linked to the appropriate administration of the "hero's dose." A dose insufficient to reach the necessary concentration will fail to elicit the desired response, while an excessively high dose can lead to detrimental side effects. The precise balance is essential.
Consider the treatment of a bacterial infection. Administering an inadequate dose of antibiotics fails to eradicate the infection, allowing bacteria to persist and potentially develop resistance. Conversely, an overly high dose of antibiotics can cause significant harm to the patient's gut microbiome and increase the risk of adverse reactions. The "hero's dose" in this context lies in identifying the minimum effective dose necessary to effectively eliminate the bacteria without producing unacceptable side effects. Similarly, in chemotherapy, the "hero's dose" represents a carefully calibrated dose of cytotoxic drugs that effectively targets cancerous cells while minimizing harm to healthy tissue. The therapeutic effect, in this case, is the successful eradication of cancerous cells, while the "hero's dose" is the precise dosage ensuring this effect while minimizing side effects like nausea and hair loss.
Understanding the relationship between therapeutic effect and the "hero's dose" is crucial for effective treatment and patient safety. Properly determining the "hero's dose" is essential to maximizing the therapeutic effect while minimizing toxicity. This requires careful consideration of individual patient characteristics, such as age, weight, and pre-existing conditions. Clinical trials and extensive research are necessary to determine optimal dosage ranges and personalize treatment protocols. Further refinement of pharmacodynamic and pharmacokinetic models promises a more nuanced understanding of drug-patient interactions, ultimately leading to even more precise and effective therapeutic strategies. This precision in identifying the "hero's dose" directly translates into optimizing patient outcomes and promoting overall well-being.
3. Patient Safety
Patient safety is paramount in medical practice, directly interwoven with the concept of the "hero's dose." Precisely determining the appropriate medication dosage, a cornerstone of the "hero's dose," is intrinsically linked to minimizing potential harm to patients. The pursuit of optimal therapeutic outcomes must always be balanced against the risk of adverse effects.
- Dose-Related Toxicity
Medication dosages, if not carefully calibrated, can induce adverse reactions ranging from mild discomfort to severe toxicity. The "hero's dose" aims to deliver the therapeutic effect with minimal toxicity. Understanding the relationship between dosage and adverse events is crucial in establishing safe treatment protocols. For example, incorrect dosages of chemotherapy drugs can lead to life-threatening organ damage, highlighting the critical need for meticulous dosage control. Overdosing on certain medications can trigger severe allergic reactions or cardiac complications. Appropriate monitoring and careful adjustment of dosage regimens are paramount in minimizing these risks.
- Individual Patient Variability
Patients exhibit a spectrum of responses to medications due to factors such as genetics, pre-existing conditions, and physiological variations. The "hero's dose," therefore, must be approached with individualization in mind. A dosage effective for one patient might be toxic for another. Precise clinical assessments and careful monitoring of individual patient responses are essential for adjusting the dosage to optimize therapeutic efficacy and minimize harm. This adaptability in dosing ensures patient safety in the face of individual variability, reflecting the personalized nature of modern medicine.
- Medication Interactions
Patients often take multiple medications simultaneously. Understanding potential drug interactions is crucial for patient safety. The "hero's dose" of one medication might be affected by concomitant medications, potentially increasing toxicity or diminishing therapeutic efficacy. Thorough review of a patient's entire medication regimen is essential for predicting and preventing adverse events. Medication interactions could lead to unintended side effects or even life-threatening consequences. The "hero's dose" must therefore consider potential interactions to ensure patient safety during multiple medication use.
- Monitoring and Adjustments
Regular monitoring of patients receiving medication is essential to track the therapeutic effect and detect any adverse reactions promptly. Continuous assessment enables real-time adjustments to the "hero's dose" if necessary. Early identification of adverse reactions allows for immediate intervention, preventing escalation of harm. Close monitoring of blood levels, symptoms, and other vital signs allows for rapid adjustments in dosage to maintain the therapeutic effect while avoiding harmful side effects. This adaptive approach to dosing is critical for maintaining patient safety throughout treatment.
In conclusion, patient safety is inextricably linked to the careful determination of the "hero's dose." A holistic approach that integrates factors like patient variability, medication interactions, and continuous monitoring is essential to ensure that treatment remains effective while minimizing potential risks. This proactive safeguarding of patient well-being underscores the importance of meticulous practice in the clinical setting, underscoring the vital role of the "hero's dose" in protecting patients from harm.
4. Reduced Toxicity
Reduced toxicity is a critical component of the "hero's dose" concept. The "hero's dose" represents the precise amount of medication necessary to achieve a therapeutic effect while minimizing harmful side effects. Minimizing toxicity is not an afterthought; it's integral to the concept. A drug's toxicity profile directly influences the determination of its optimal dose. Lower doses generally correspond to lower potential for adverse reactions, while higher doses increase the likelihood of toxicity. Careful consideration of the drug's toxicity profile is paramount in identifying the "hero's dose." This principle underpins many successful clinical treatments. For instance, in cancer chemotherapy, the "hero's dose" aims to effectively target cancerous cells while minimizing harm to healthy tissue. The focus on reduced toxicity directly impacts treatment efficacy and patient well-being. The goal is not just to eradicate the disease but also to ensure patient survivability and quality of life.
Practical applications of this concept are evident across diverse medical fields. In treating chronic conditions like hypertension, medications are chosen and dosed to control blood pressure effectively with minimal risk of adverse effects. Lower doses of potentially toxic medications, carefully calibrated, ensure optimal therapeutic outcomes without unnecessary harm. The development of targeted therapies, drugs designed to specifically interact with diseased cells, demonstrates a commitment to minimizing systemic toxicity, thereby increasing treatment efficacy and reducing the potential for broad-spectrum side effects. In each case, the emphasis on reduced toxicity within the "hero's dose" paradigm reflects a proactive approach to ensuring patient well-being. Drug development now increasingly emphasizes identifying drugs with a higher therapeutic index (ratio of toxic dose to therapeutic dose). A wider therapeutic index indicates a larger safety margin, allowing for a wider range of effective doses while minimizing toxicity.
In summary, reduced toxicity is inseparable from the "hero's dose." Finding the optimal dosage involves meticulous consideration of the drug's potential toxicity. This is not simply about avoiding harm; it's about maximizing therapeutic benefit while minimizing potential harm. While challenges such as inter-patient variability and drug interactions persist, the focus on reduced toxicity remains central to the advancement of safer and more effective treatments. By prioritizing reduced toxicity in the context of the "hero's dose," medical practice aims to achieve optimal therapeutic outcomes with minimal risk to patients.
5. Clinical Trial Design
Clinical trial design plays a critical role in determining the "hero's dose" of a medication. The process involves meticulously planning and executing experiments to evaluate a drug's efficacy and safety. Trial design dictates the methodology for selecting participants, administering the drug, measuring outcomes, and analyzing results. Crucially, the design must effectively identify the optimal dosage range for the drug. A poorly designed clinical trial can result in an inaccurate estimation of the "hero's dose," leading to suboptimal treatment or potential harm.
Several key elements within clinical trial design directly influence the determination of the "hero's dose." The study's participant selection criteria are paramount. Researchers must carefully define inclusion and exclusion criteria to ensure the study population accurately reflects the intended patient population. This stratification ensures that results are generalizable and applicable to the target patient group. The dosage regimen employed within the trial is fundamental. The trial design should outline a systematic escalation of doses, progressing from low to potentially higher doses. This allows researchers to observe responses at various dosage levels, crucial for identifying the optimal range. This approach, coupled with careful monitoring for adverse events at each dosage level, allows for the determination of the dose associated with the most favorable benefit-to-risk ratio. Standardized procedures for data collection and analysis are essential for ensuring accurate and reliable results. Rigorous data collection methods help reduce bias and improve the reliability of the findings, thus influencing the confidence with which the optimal dose is determined. The trial design should also factor in appropriate control groups, placebo groups, or comparisons with existing treatments. This helps accurately assess the medication's effectiveness relative to other options. Careful consideration of these design aspects allows researchers to define the optimal dose range, leading to safer and more effective treatments. For instance, a well-designed clinical trial for a new cancer drug might establish a dosage regime of escalating doses of the drug in participants, comparing responses to the targeted cancer cells with minimal adverse effects on healthy tissue. This rigorous approach ensures a precise definition of the "hero's dose," maximizing efficacy and safety.
In conclusion, sound clinical trial design is essential for establishing the "hero's dose" of a medication. A well-structured trial, addressing participant selection, dosage regimen, data collection, and analysis, is crucial to ensuring accurate and reliable results. The design directly influences the confidence with which the optimal dosage is determined. Precisely determining the "hero's dose" improves patient outcomes by maximizing treatment efficacy while minimizing potential harm. Ethical considerations and adherence to regulatory guidelines are vital throughout the trial design and execution process. These principles are essential not only for the development of new treatments but also for improving existing ones, thereby contributing to the broader goal of promoting patient safety and health.
6. Individualized Treatment
Individualized treatment, a cornerstone of modern medicine, necessitates tailoring therapeutic approaches to the unique characteristics of each patient. This approach directly impacts the concept of the "hero's dose." The optimal dosage for a given medication isn't a universal constant but varies significantly based on individual factors. A single dose regimen may be ineffective or even harmful for some patients while proving beneficial for others. This variability highlights the importance of individualized treatment as a crucial component of determining the "hero's dose." Ultimately, the "hero's dose" is not a fixed value but a range tailored to the specific patient.
Factors influencing individualized treatment and, consequently, the "hero's dose," include genetics, physiology, metabolism, and pre-existing conditions. Genetic variations impact how patients metabolize medications, influencing drug efficacy and potential toxicity. Patients with impaired liver or kidney function, for instance, may require lower doses to prevent accumulation of potentially harmful drug metabolites. Furthermore, the patient's overall health status, including comorbidities, can significantly alter the appropriate dosage. A patient with a pre-existing heart condition, for example, might necessitate a lower dose of a particular medication than a healthy individual. Acknowledging these variations allows for the careful calibration of the "hero's dose" to maximize therapeutic benefits while minimizing risks. Consider a patient with a known allergy to a medication componenta universal dose might trigger a severe reaction, rendering individualized dosage critical for patient safety. The treatment plan must adapt to accommodate these individual needs.
The practical significance of this understanding extends beyond individual patient safety. In clinical trials, recognizing individual variability allows for more accurate estimations of the "hero's dose" for a given population. Pooling data from heterogeneous populations without accounting for individual factors can produce inaccurate results, potentially leading to suboptimal treatments or, worse, to adverse events. By meticulously considering and incorporating individual factors, the determination of the optimal dose range becomes more precise, leading to better treatment outcomes. Consequently, individualized treatment empowers a more precise, personalized approach to managing chronic diseases, improving overall treatment efficacy, and minimizing potential harm. This precision is paramount in conditions like cancer treatment, where tailored approaches based on tumor characteristics and patient response are increasingly recognized as essential for successful outcomes. The broader goal is the development of safer and more effective treatments for a wider spectrum of patients.
7. Drug Efficacy
Drug efficacy, the ability of a medication to produce a desired therapeutic effect, is intrinsically linked to the "hero's dose." The optimal dose, often referred to as the "hero's dose," is not arbitrarily chosen; it's meticulously determined to maximize the drug's beneficial effects while minimizing potential harm. A drug's efficacy directly correlates with the appropriate dose. An insufficient dose fails to achieve the desired therapeutic response, while an excessively high dose may induce adverse effects. Therefore, precise dosage is critical for achieving optimal drug efficacy. This relationship is foundational in determining the most effective and safest treatment strategies.
Consider the treatment of hypertension. A medication effective in lowering blood pressure requires a specific dosage. An insufficient dose might not sufficiently reduce blood pressure, rendering the treatment ineffective. Conversely, a dose exceeding the optimal level could lead to adverse reactions, diminishing the treatment's efficacy and potentially jeopardizing patient safety. The optimal dose thus balances therapeutic effect and safety. In cancer therapy, a drug effective in targeting cancerous cells requires an appropriate dosage. A suboptimal dose may not adequately eliminate the tumor, while an excessively high dose might damage healthy tissues. The "hero's dose" in this context represents the precise balance that maximizes the drug's anti-cancer effect while minimizing toxicity to healthy cells. This concept directly influences the choice of treatment and impacts patient outcomes.
Understanding the connection between drug efficacy and the "hero's dose" is vital for the development and application of effective therapies. Clinical trials meticulously explore the dose-response relationship to identify the optimal dosage range, maximizing the therapeutic effect and minimizing adverse events. This knowledge is essential for designing personalized treatment strategies, as individual patient responses to medications vary significantly. Factors like metabolism, genetics, and pre-existing conditions influence drug efficacy and toxicity. Precisely determining the "hero's dose" allows for a more tailored approach to treatment, ensuring that each patient receives the most effective and safest dose. This understanding emphasizes the importance of rigorous research and careful consideration of individual patient variables in maximizing treatment outcomes while minimizing harm.
8. Minimizing Side Effects
Minimizing adverse effects is an integral component of the "hero's dose" concept. A "hero's dose" is not simply the highest effective dose but the precise dose that yields the desired therapeutic effect with the least potential for undesirable side effects. This meticulous approach reflects a fundamental principle in pharmacology: maximizing therapeutic benefit while minimizing harm. The connection is direct and consequential. A dose too high can overwhelm the body's physiological systems, triggering adverse responses, potentially leading to severe complications. Conversely, an inadequate dose may fail to achieve the intended therapeutic outcome. The "hero's dose" strives for the optimal balance. Understanding this relationship is critical for safe and effective treatment regimens.
Consider chemotherapy treatments for cancer. High doses of chemotherapeutic agents are often necessary to combat rapidly dividing cancer cells, but these same agents can harm healthy cells, leading to debilitating side effects such as nausea, hair loss, and weakened immune systems. The "hero's dose" in this context involves carefully selecting and administering the minimal effective dose capable of targeting cancerous cells while minimizing the damage to healthy tissue. This meticulous approach is vital for patient survival and quality of life during and after treatment. In treating cardiovascular conditions, a similar principle applies. Medications designed to lower blood pressure, for example, must be dosed precisely to achieve the desired blood pressure reduction without causing excessive side effects like dizziness or orthostatic hypotension. Determining the "hero's dose" in these cases involves a careful balancing act, aiming to maximize efficacy while minimizing potential complications.
The practical significance of minimizing side effects within the framework of the "hero's dose" is profound. Precise dosage not only improves patient outcomes but also enhances treatment adherence. Patients are more likely to continue a prescribed regimen if the side effects are tolerable. This improved adherence significantly increases the likelihood of achieving therapeutic goals. Furthermore, reducing side effects contributes to a better quality of life for patients undergoing treatment. The "hero's dose," therefore, encompasses more than just effectiveness; it signifies a commitment to patient well-being. While challenges such as inter-individual variability and drug interactions persist, ongoing research continues to refine methods for determining and administering "hero's doses" with maximum therapeutic benefits and minimal adverse effects. This ongoing effort underscores the commitment to responsible and effective medical practice.
Frequently Asked Questions about "Hero's Dose"
This section addresses common inquiries regarding the concept of "hero's dose" in medical practice. Accurate understanding of this crucial pharmacological principle is essential for patient safety and effective treatment.
Question 1: What exactly is a "hero's dose"?
A "hero's dose" is not a universal dosage but rather the precise, optimal amount of medication calculated to achieve the desired therapeutic effect while minimizing potential harm. This calculated dosage balances efficacy with safety, aiming for the most effective treatment with the fewest side effects. It represents the minimum effective dose. Crucially, it varies significantly based on individual patient factors.
Question 2: How is the "hero's dose" determined?
Determining the "hero's dose" is a complex process involving clinical trials, rigorous research, and extensive data analysis. Factors considered include the drug's pharmacokinetic properties (how the body absorbs, distributes, metabolizes, and excretes the drug), patient-specific characteristics (age, weight, pre-existing conditions), and potential interactions with other medications. Pharmacogenomics and biomarkers are increasingly used to refine individualized dosing strategies.
Question 3: Is a "hero's dose" always the largest effective dose?
No. A "hero's dose" is the lowest effective dose that produces the desired therapeutic outcome without triggering unacceptable side effects. It represents a carefully calculated balance, not a maximal dose. The key is minimizing potential harm while maximizing the treatment's effectiveness.
Question 4: How does the "hero's dose" relate to patient safety?
The "hero's dose" is intrinsically linked to patient safety. Precisely identifying this dose minimizes the risk of adverse reactions, from mild discomfort to severe toxicity. Careful consideration of individual patient characteristics ensures the treatment is effective and safe, minimizing potential harm.
Question 5: How do clinical trials contribute to determining the "hero's dose"?
Clinical trials are essential for establishing the "hero's dose." These controlled experiments rigorously evaluate the drug's effectiveness and safety at various dosages. The data generated from these trials allows researchers to determine the optimal dose range, minimizing risk and maximizing therapeutic benefit. The results guide appropriate dosing protocols for diverse patient populations.
In summary, the "hero's dose" represents a carefully calculated and tailored approach to medication administration. Its determination involves a complex interplay of factors, including pharmacological properties, patient-specific characteristics, and potential interactions. The goal is to maximize treatment efficacy while minimizing potential adverse effects and ensuring patient safety.
This concludes the frequently asked questions about the "hero's dose." For specific inquiries or personalized advice, consult a qualified healthcare professional.
Conclusion
The exploration of the "hero's dose" reveals a multifaceted concept central to modern medical practice. Determining the optimal dosage for a medication is not a simple calculation but a complex process requiring meticulous consideration of numerous factors. Precise dosage hinges on understanding a drug's pharmacological profile, including its efficacy, potential toxicity, and pharmacokinetic properties. Furthermore, individual patient variability, including genetic predispositions, physiological differences, and pre-existing conditions, necessitates tailored approaches. Clinical trial design plays a critical role in establishing safe and effective dosage ranges, ensuring the balance between therapeutic benefit and potential harm. The concept underpins personalized medicine, where treatment strategies are adapted to individual patient needs. Ultimately, the "hero's dose" embodies the delicate balance required for effective therapies that prioritize patient safety while maximizing treatment outcomes. This approach is crucial for responsible and effective medical practice.
The pursuit of the "hero's dose" underscores the continuous need for advancements in medical research and technology. Continued exploration into pharmacogenomics, personalized medicine, and refined methodologies for clinical trials will further refine the identification and application of optimal dosages. A deeper understanding of the complexities inherent in drug interactions and individual patient responses will lead to even safer and more efficacious treatments. The future of medicine hinges on the accurate and responsible application of the principles underpinning the "hero's dose," ultimately leading to improved patient care and outcomes.
- Best Panama Bakeries Amp Pastries Freshly Baked Delights
- Arsenal Training Gooner Academy Expert Coaching
/what-is-a-k-hole-21861_FINAL-5bd0bf8ac9e77c0051074e07.png)